What is Ovarian Health? A Complete Guide to Understanding and Supporting It
Let's cut through the noise. When you hear "ovarian health," you might think about periods, maybe babies, or even scary words like cancer. But that's selling it short. In my years talking with patients and diving into the research, I've seen how reducing it to just fertility does a disservice to every woman. Ovarian health is the cornerstone of your entire endocrine orchestra. It's about sustainable energy, stable moods, strong bones, a sharp brain, and yes, the potential for life. When your ovaries are functioning well, they do more than release an egg—they regulate a symphony of hormones that touch every cell in your body.
Ignoring it until you hit a wall—like painful periods that floor you or trouble conceiving—is the most common mistake I see. The goal isn't to obsess, but to understand. Knowledge lets you spot subtle shifts early and become an active partner in your own care, not just a passenger.
In This Article
Beyond the Egg: What Ovarian Health Really Means
Think of your ovaries as a master gland, not just a storage unit. Their core job is twofold: gamete production (making and releasing eggs) and steroidogenesis (producing hormones, primarily estrogen and progesterone).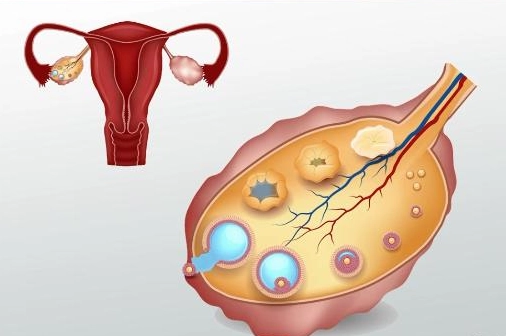
But here's the part most articles gloss over: the quality of these functions matters more than just their existence. You can be ovulating monthly but if the hormonal communication is off—like a weak luteal phase with low progesterone—it can affect everything from sleep quality to anxiety levels, long before fertility becomes a question.
A Non-Consensus View: Many think a regular period equals perfect ovarian health. Not necessarily. I've seen women with clockwork cycles who have undiagnosed ovulatory dysfunction (they release an egg, but the hormonal support is subpar). The cycle is a report card, and you need to read beyond just the due date.
The Three Key Pillars of Ovarian Function
To truly grasp it, break it down into these three interconnected pillars.
1. Hormonal Rhythm and Balance
This isn't about static levels. It's about the dynamic dance between estrogen, progesterone, follicle-stimulating hormone (FSH), and luteinizing hormone (LH) across your cycle. Estrogen builds you up (energy, mood, lining), progesterone calms and maintains. A healthy ovary responds precisely to signals from the brain and creates a balanced, timely output.
When this rhythm is off, you might feel it as brutal PMS, mid-cycle spotting, or a heavy, clot-filled period—all signs the hormonal conversation is noisy.
2. Ovarian Reserve and Follicular Health
Your ovarian reserve is your pool of potential eggs (primordial follicles). Quantity naturally declines with age, but quality is heavily influenced by lifestyle. Each follicle is a tiny ecosystem. Oxidative stress from pollution, smoking, or poor diet damages that ecosystem, affecting the egg's viability and the follicle's ability to produce good hormones.
3. Structural and Anatomical Integrity
Healthy ovaries are free of large cysts that disrupt function, endometriosis implants, or scar tissue (adhesions) that can strangle blood supply or distort anatomy. Recurrent ovarian cysts aren't always "bad luck"; they can signal an underlying hormonal imbalance that needs addressing.
Warning Signs: When Your Ovaries Might Be Calling for Help
Your body sends memos before it sends emergency alerts. Don't ignore these.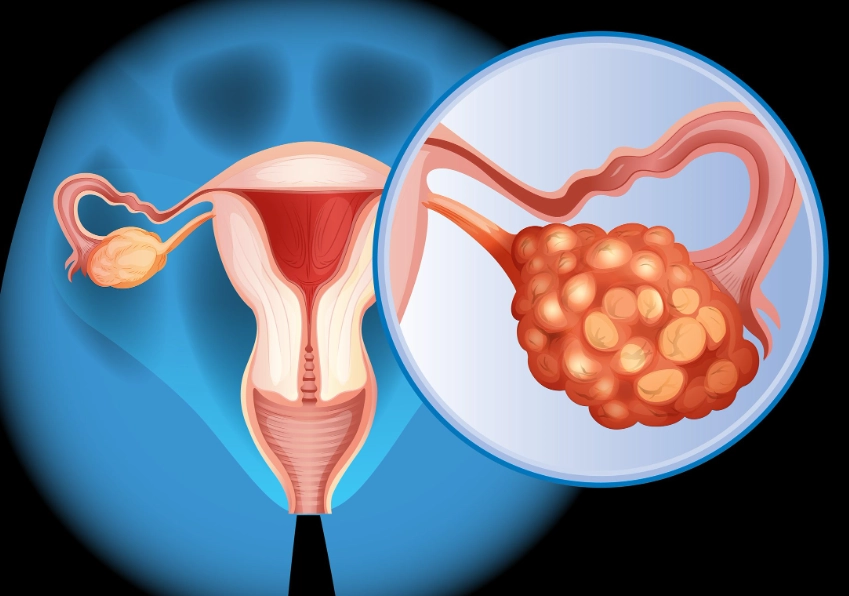
| Sign or Symptom | What It Might Indicate | Action Step |
|---|---|---|
| Major cycle changes (cycle shortening | Possible anovulation, PCOS, perimenopause, thyroid issues. | Start cycle tracking. See a doctor if pattern persists for 3 cycles. |
| Severe PMS or PMDD that disrupts your life | Potential progesterone sensitivity, estrogen dominance, nutrient deficiencies. | Track specific symptoms. Review diet/stress. Discuss with a gynecologist. |
| Painful periods (Dysmenorrhea) beyond mild cramping | Could be normal, but can signal endometriosis, adenomyosis, or fibroids. | Don't just "tough it out." Pain that requires strong meds or misses work needs investigation. |
| Very heavy bleeding (soaking a pad/tampon in | Hormonal imbalance (often low progesterone), fibroids, polyps. | Rule out structural issues with an ultrasound. Check iron levels. |
| Missing ovulation signs (no cervical mucus change, no mild mid-cycle pain) | Anovulatory cycles, common in PCOS, stress, low body weight. | Learn to chart your cycle (temperature, mucus). Bring data to your doctor. |
Red Flags Requiring Prompt Medical Attention: Sudden, severe pelvic pain; pain with fever; bleeding after menopause; or rapid, unexplained abdominal bloating. These are not "wait and see" situations.
Your Action Plan: How to Support Ovarian Health Proactively
This isn't about drastic overhauls. It's about consistent, smart support.
Nutrition: Fuel for the Follicles
Forget fad diets. The Mediterranean diet pattern wins for a reason. Focus on:
Colorful antioxidants: Berries, leafy greens, nuts. They combat oxidative stress in follicles.
Healthy fats: Avocado, olive oil, fatty fish. Cholesterol is the raw material for your sex hormones.
Complex carbs & fiber: Whole grains, legumes. They modulate insulin and help excrete excess estrogen.
Key nutrients: Choline (eggs), magnesium (pumpkin seeds, spinach), and zinc (seafood, lentils).
I once worked with a woman whose cycles were all over the place. We simply added a serving of lentils and a handful of walnuts daily, and focused on consistent breakfasts. Her cycles regulated within three months. It wasn't magic—it was stabilizing blood sugar and providing building blocks.
Movement: The Sweet Spot
Extreme exercise can suppress ovulation. The goal is moderate, regular movement that reduces inflammation and improves insulin sensitivity: brisk walking, cycling, yoga, strength training. If your period disappears with intense training, that's a clear sign from your ovaries to dial it back.
Stress and Sleep: The Non-Negotiables
Chronic stress elevates cortisol, which can literally steal the precursors needed to make progesterone. It tells your body, "Now is not a safe time for reproduction." Prioritizing 7-8 hours of sleep and finding a daily de-stress practice (10 minutes of deep breathing, a walk in nature) isn't fluffy self-care—it's direct hormonal support.
Environmental Toxins: A Practical Approach
You can't avoid everything, but you can reduce major exposures. Swap plastic food containers for glass or stainless steel. Choose fragrance-free personal care products when possible. Filter your drinking water. These endocrine disruptors (like BPA and phthalates) can mimic or block hormones, muddying the signals to your ovaries.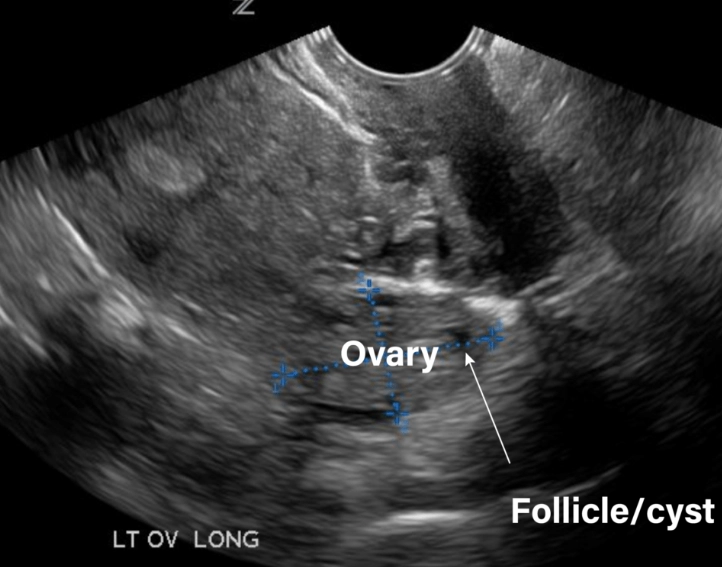
The Medical Corner: Tests and When to Seek Help
Knowledge is power, especially when you bring it to a doctor's appointment.
When to see a doctor: If you have any of the warning signs for more than 2-3 cycles, if you're under 35 and have been trying to conceive for a year without success (6 months if over 35), or if you have a family history of early menopause or ovarian cancer.
Key diagnostic tests your doctor might use:
Cycle Day 3 Hormone Panel: Checks FSH, LH, Estradiol to assess ovarian reserve and function.
Anti-Müllerian Hormone (AMH): Another reserve indicator, but remember—it's just one piece.
Transvaginal Ultrasound: Looks at ovarian volume, antral follicle count (AFC), and checks for cysts or abnormalities.
Thyroid Panel (TSH, Free T4): Thyroid issues masquerade as ovarian problems.
Organizations like the American College of Obstetricians and Gynecologists (ACOG) provide excellent patient resources on these topics. For research on conditions like PCOS, the American Society for Reproductive Medicine (ASRM) is a reliable source.
Your Burning Questions Answered
So, what is ovarian health? It's the dynamic, foundational piece of your biological well-being that influences far more than your reproductive plans. It's a system to be understood and supported through daily choices, not feared or ignored. Start by paying closer attention to your cycle's unique language. Make one or two supportive tweaks to your routine. And remember, you don't need a problem to start being proactive. Building resilience in this core system pays dividends for your vitality at every stage of life.
POST A COMMENT