How to Know Your Menstrual Cycle Phase: A Complete Guide
You look at your calendar and wonder, "What phase of my cycle am I in right now?" Maybe you're trying to conceive, aiming to avoid pregnancy naturally, or just want to understand why you feel a certain way. The answer isn't just a date on an app. It's written in the subtle, daily signals from your body.
Knowing your menstrual cycle phases is like having an owner's manual for your hormones. It empowers you. Let's cut through the confusion and talk about how you can figure it out for yourself, reliably.
What's Inside This Guide
The Four Phases of Your Cycle: A Roadmap
Forget the idea of a "28-day cycle" as the gold standard. Normal is a range, typically 21 to 35 days. The phases, however, follow a consistent hormonal script. Think of your cycle in two main acts, divided by ovulation.
Act 1: The Follicular Phase (Pre-Ovulation)
This phase starts on day 1 of your period and ends at ovulation. Estrogen is the star here, slowly rising to build up your uterine lining and mature an egg.
- Menstruation (Days 1-5ish): The cycle's reset. Estrogen and progesterone are at their lowest. You bleed.
- Post-Period, Pre-Ovulation: After bleeding stops, estrogen climbs. Energy often increases, mood may lift, and cervical fluid starts to change from dry or sticky to creamy.
The Main Event: Ovulation
This isn't a phase, but the pivotal 24-hour window when a mature egg is released. A surge of Luteinizing Hormone (LH) triggers it. Estrogen peaks right before. This is your fertile peak.
Act 2: The Luteal Phase (Post-Ovulation)
This phase lasts from ovulation until the day before your next period. It's more fixed in length, usually 10-16 days (14 is common). Progesterone takes over to support a potential pregnancy.
If no pregnancy occurs, progesterone and estrogen fall, triggering your next period. This hormone drop is often responsible for Premenstrual Syndrome (PMS) symptoms like mood swings, bloating, and breast tenderness.
| Phase | Key Hormone | Typical Length | What's Happening |
|---|---|---|---|
| Menstrual | Low Estrogen & Progesterone | 3-7 days | Uterine lining sheds. Period begins. |
| Follicular | Rising Estrogen | ~7-21 days (varies most) | Egg matures. Lining rebuilds. Energy often rises. |
| Ovulation | LH & Estrogen Surge | ~24 hours | Egg is released. Peak fertility. |
| Luteal | High Progesterone | 10-16 days (often 14) | Body preps for pregnancy. PMS symptoms may appear. |
How to Identify Your Cycle Phase: The Body's Clues
Your body gives you tangible signs. You just need to know what to look for. The two primary biomarkers are cervical fluid and basal body temperature.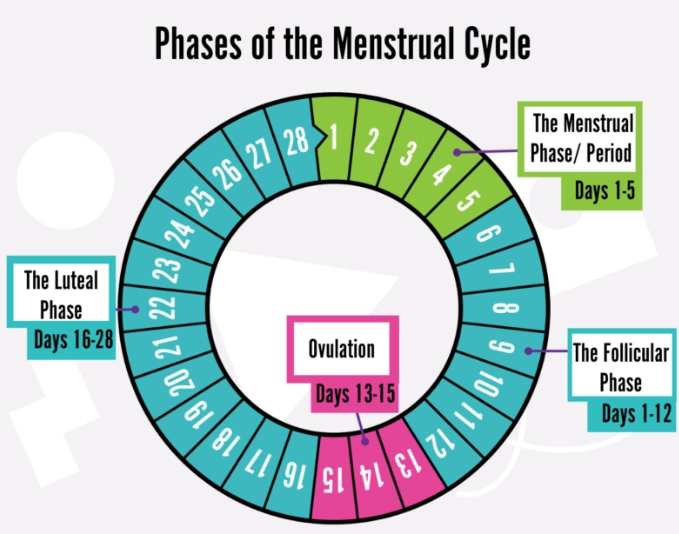
1. Cervical Fluid (Mucus): Your Fertility Litmus Test
This is the most immediate sign. Its quality changes in direct response to estrogen.
- Menstruation: Blood masks the fluid.
- Early Follicular (post-period): Often dry or sticky. Little to no fluid.
- Approaching Ovulation: Fluid becomes creamy, lotion-like, white or cloudy.
- Peak Fertile (Ovulation): The classic sign. Fluid is clear, stretchy, slippery, and resembles raw egg white. It can stretch between your fingers without breaking. This creates a conducive environment for sperm.
- Post-Ovulation (Luteal Phase): Fluid dries up quickly, becoming sticky or dry again, or you may feel a persistent dampness without the slippery quality.
Check it at the same time daily (like when you go to the bathroom). Observe the sensation at the vaginal opening and the quality on toilet paper or your fingers.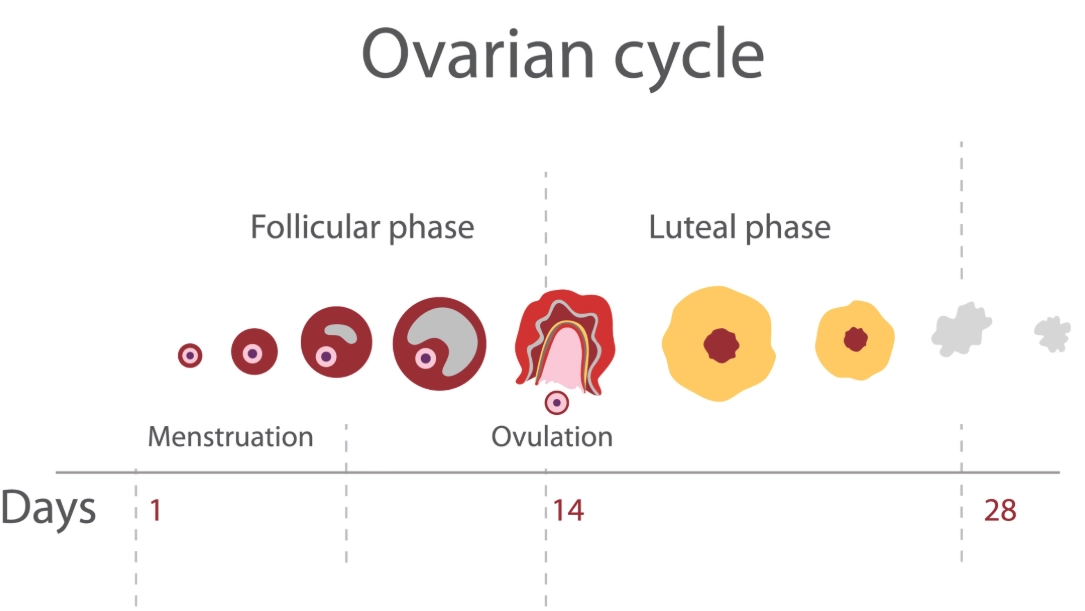
2. Basal Body Temperature (BBT): The Confirmation Signal
BBT is your body's temperature at complete rest. Progesterone, released after ovulation, causes a slight but sustained rise (about 0.5-1 degree Fahrenheit).
The Pattern: Your temperatures will be lower during the follicular phase. After ovulation, they shift to a higher range and stay elevated until your next period. The shift confirms ovulation has occurred. It's a retrospective sign, not a predictor.
You need a sensitive basal thermometer (two decimals) and must take your temperature immediately upon waking, before sitting up or talking. Consistency is non-negotiable.
3. Secondary Signs: The Supporting Cast
These vary from person to person but add valuable context.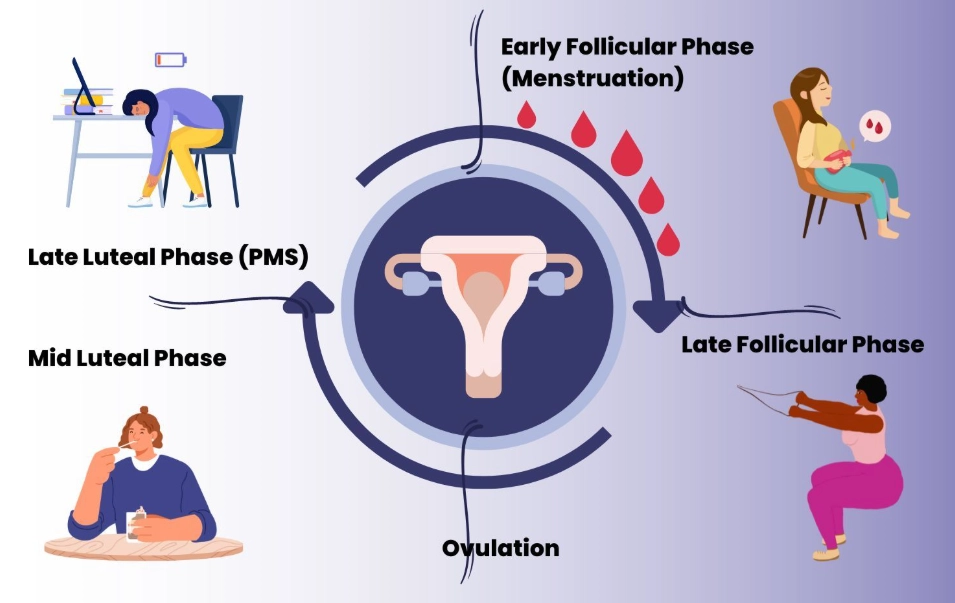
- Cervical Position: Around ovulation, the cervix becomes high, soft, and open (like your lips). Post-ovulation, it becomes low, firm, and closed (like the tip of your nose). This takes practice to discern.
- Ovulation Pain (Mittelschmerz): A brief, one-sided twinge or ache around ovulation time.
- Libido: Often peaks around ovulation due to high estrogen.
- Breast Tenderness: Common in the luteal phase due to progesterone.
- Mood & Energy: Many feel more energetic and social in the follicular phase, and more inward-focused or irritable in the luteal phase.
Putting It All Together: Effective Tracking Methods
Now, how do you log and interpret these signs? Here are your main options.
Option 1: Pen-and-Paper Charting
The classic method used in systems like the Symptothermal Method (taught by organizations like Fertility UK). You note daily BBT, cervical fluid quality, and other signs on a paper chart. It's highly educational and avoids app algorithms.
Option 2: Dedicated Cycle Tracking Apps
Apps like Kindara, Read Your Body, or Ovia Fertility allow you to input your biomarkers. The good ones don't just predict; they let you record your observations and learn your pattern. Avoid apps that only use calendar predictions.
Let's follow Sarah, who has a 32-day cycle. On cycle day 10, her app might predict ovulation soon based on averages. But Sarah notices only creamy cervical fluid and her BBT is still low. By day 16, she sees egg-white fluid. She logs it. On day 18, her BBT spikes and stays up. The app now confirms ovulation based on her data, not a guess. She knows she's in the luteal phase.
Option 3: Ovulation Predictor Kits (OPKs)
These urine tests detect the LH surge that precedes ovulation by 24-36 hours. They're great for pinpointing your fertile window, especially if cervical fluid is tricky to observe. They tell you ovulation is coming, but BBT confirms it happened.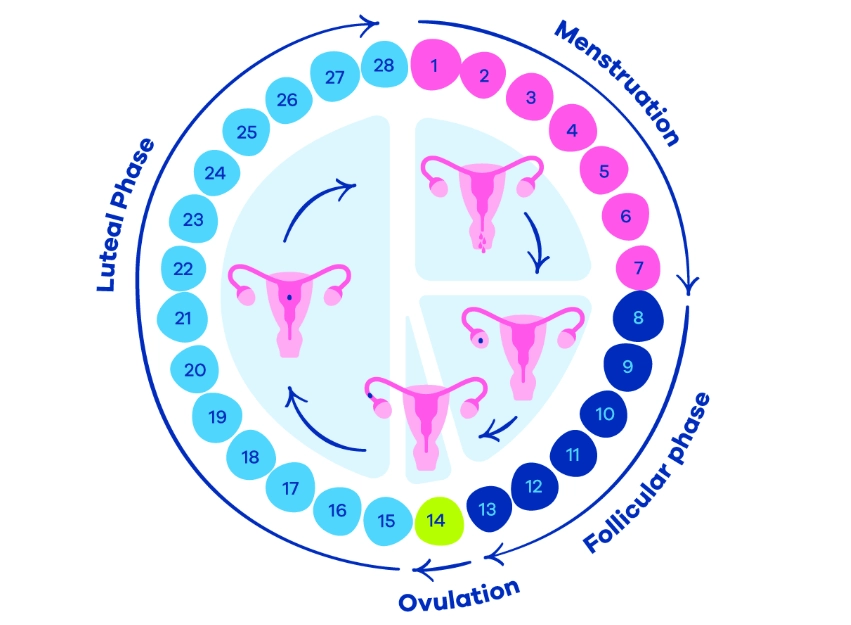
A crucial nuance most miss: A positive OPK means your body is trying to ovulate. It doesn't guarantee the egg is released (this is called an anovulatory cycle). That's why pairing an OPK with BBT or cervical fluid confirmation is the gold standard for certainty.
Common Mistakes in Cycle Tracking (And How to Avoid Them)
After a decade of tracking and coaching others, I see the same pitfalls repeatedly.
Mistake 1: Relying Solely on a Calendar App. These apps use population averages and your past data to guess. They know nothing about your body's signals this cycle. Stress, illness, or travel can shift ovulation, rendering the prediction useless. Use them as a digital notebook, not an oracle.
Mistake 2: Inconsistent BBT Timing. Taking your temperature at 6 AM one day and 8 AM the next introduces noise. A consistent wake-up time is ideal, but if you wake earlier or later on weekends, still take it immediately. Note the time. Some apps (like Femometer) have algorithms to adjust for this.
Mistake 3: Misreading Cervical Fluid. Confusing arousal fluid (which is transient) with fertile-quality fluid is common. Arousal fluid is often more watery and dissipates quickly. True egg-white fluid persists throughout the day and has that distinctive stretchiness. Also, semen can mimic fertile fluid for several hours after intercourse.
Mistake 4: Starting to Track When You Have a Goal. If you're trying to conceive or avoid pregnancy, start tracking for at least 3 full cycles beforehand. This gives you time to learn your unique patterns without pressure. You'll make mistakes in the learning phase—better to make them when the stakes are low.
Your Cycle Tracking Questions, Answered
Figuring out "what phase of my cycle am I in?" transforms from a mystery into a daily conversation with your body. It's not about achieving perfect charts. It's about paying attention. Start with one sign—maybe just checking your cervical fluid for a month. Then add BBT. Be curious, not critical. The knowledge you gain is lifelong and deeply empowering.
POST A COMMENT