Ovarian Disorder Symptoms: Your Comprehensive Guide to Detection
I remember a patient, Sarah, who came in convinced she had a persistent gluten intolerance. She'd been living with bloating, vague stomach aches, and feeling full after a few bites for nearly a year. Her primary care doctor ran GI tests, which came back normal. It wasn't until she mentioned her periods had become slightly more painful that we did a pelvic ultrasound. She had a sizable ovarian cyst. Her story isn't rare. Ovarian disorders often masquerade as other, more common ailments. The symptoms whisper; they rarely shout. And learning to listen to those whispers is the key to early detection.
What's Inside This Guide
The Common Symptom Threads You Can't Ignore
Ovarian issues don't happen in a vacuum. They involve a central organ that sits near your bladder, colon, and major blood vessels. When something's off, the symptoms often reflect that neighborhood. They're frustratingly non-specific, which is why they get missed. But when several show up together and persist for more than a few weeks, that's your cue to look deeper.
Let's break down the major players:
Pelvic and Abdominal Sensations: More Than Just a Bad Period
This isn't your standard menstrual cramp. We're talking about a dull ache, a heavy feeling, or a pressure that sits low in your pelvis. It might be constant, or it might come and go. Some women describe it as a feeling of "something being there." For cysts, the pain can be sharp and localized to one side—ovarian cyst pain location is often a clear left or right lower abdominal pinch. A twisted ovary (torsion) causes sudden, severe, knife-like pain that sends you to the ER.
Bloating is the great imitator. The bloating linked to ovarian issues is different. It's persistent. Your pants feel tight consistently, not just after a big meal. It doesn't fully go away overnight. This is often due to fluid accumulation (ascites) or the mass of a cyst or tumor itself.
Your Digestive System Goes Haywire
This is where things get confusing. You might feel full unusually quickly when you eat (early satiety). Even a small meal makes you feel stuffed and uncomfortable. Changes in bowel habits—new constipation or diarrhea—can pop up. Nausea or indigestion that doesn't respond to typical remedies is another red flag. The ovary is literally pushing on your intestines, messing with their normal function.
Urinary Changes: It's Not Always a UTI
A new, persistent need to urinate more often, or a feeling of urgency where you have to go now, can be a sign. Pressure on the bladder from an ovarian mass reduces its capacity. The crucial detail? These symptoms don't clear up with a course of antibiotics because it's not an infection.
Menstrual and Hormonal Shifts
For disorders like PCOS, irregular, heavy, or absent periods are a hallmark. But any ovarian issue can disrupt your cycle. You might notice spotting between periods, or your periods might become more painful. For women past menopause, any vaginal bleeding is an immediate reason to see a doctor.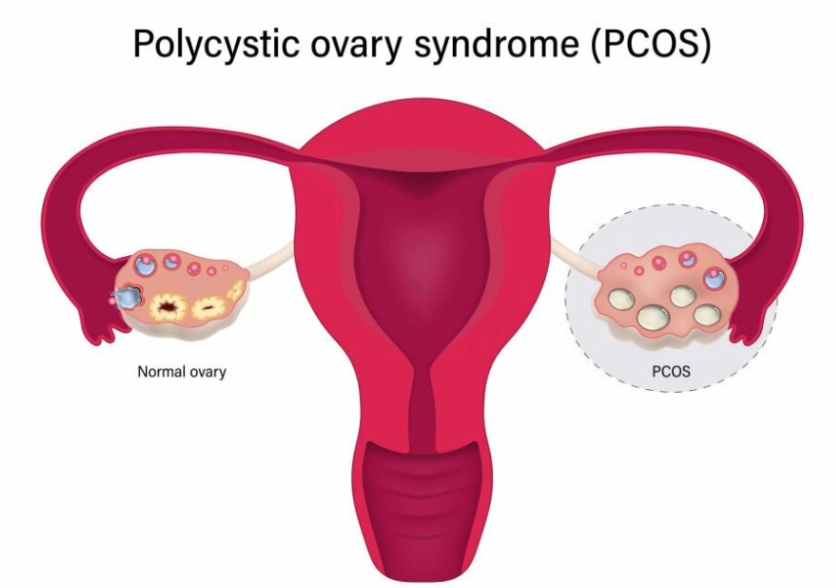
The Expert's Non-Consensus View: Most lists will tell you "bloating, pelvic pain, urinary issues." The nuance they miss? The sequence and persistence. With serious conditions like ovarian cancer, these symptoms are new (they started within the last year), they occur nearly daily, and they progressively worsen. They represent a change from your personal baseline. Tracking that timeline in a symptom diary is more valuable than any single symptom.
Symptom Breakdown: PCOS, Cysts, and Ovarian Cancer
While symptoms overlap, the emphasis and combination often point to a specific condition. This table isn't for self-diagnosis, but to help you have a more informed conversation with your doctor.
| Condition | Hallmark Symptoms | Subtle / Often Missed Signs | Typical Pain Pattern |
|---|---|---|---|
| Polycystic Ovary Syndrome (PCOS) | Irregular/absent periods, excess hair growth (hirsutism), acne, weight gain (especially around the middle), difficulty getting pregnant. | Darkening of skin in body folds (acanthosis nigricans), mood swings/anxiety, sleep apnea, severe fatigue. Hair thinning on the scalp (female pattern hair loss). A complete PCOS symptoms checklist should include these metabolic and emotional factors. | Dull, chronic pelvic ache. Cramping may be heavier during irregular periods. |
| Ovarian Cysts (Functional, Dermoid, Cystadenoma) | One-sided pelvic pain (ovarian cyst pain location is key), bloating, fullness in the lower abdomen. | Pain during intercourse, pain just before your period starts or ends, a dull ache in your lower back or thighs. A ruptured cyst causes sudden, sharp pain followed by diffuse discomfort. | Sharp, intermittent, or aching pain localized to one side. Sudden, severe pain if torsion or rupture occurs. |
| Ovarian Cancer | Persistent abdominal bloating, feeling full quickly, pelvic/abdominal pain, urinary urgency/frequency. | Unexplained fatigue, changes in bowel habits (constipation), unexplained weight loss (or gain around the abdomen), back pain. The bloating is often progressive and unrelenting. These are the critical early signs of ovarian cancer, though "early" is a relative term. | Vague, persistent discomfort or pressure. Not always severe, but always present. |
Looking at that table, you see the overlap. Sarah's "gluten intolerance" symptoms—bloating, early satiety—are right there in the ovarian cancer column. That's why context is everything.
One of the biggest mistakes I see? Women (and sometimes doctors) attribute new urinary frequency or constipation purely to aging or diet, without considering pelvic pressure as a cause. It creates dangerous delays.
What to Do If You Recognize These Signs
Don't panic, but do take action. This is a step-by-step process of advocating for yourself.
Step 1: Start a Symptom Log
For two weeks, jot down notes. Be specific. Not "felt bloated," but "Could not button work pants, feeling lasted all day." Not "had to pee," but "Woke up 3 times last night to urinate, unusual for me." Track pain location, what you ate, and your cycle. This log transforms vague complaints into clinical data.
Step 2: Schedule the Right Appointment
See a gynecologist, not just a general practitioner. A gynecologist is trained to think pelvis-first. When you call, be direct: "I have persistent pelvic bloating and pain, and I'm concerned about my ovarian health. I'd like a pelvic exam and to discuss an ultrasound." This frames the visit appropriately.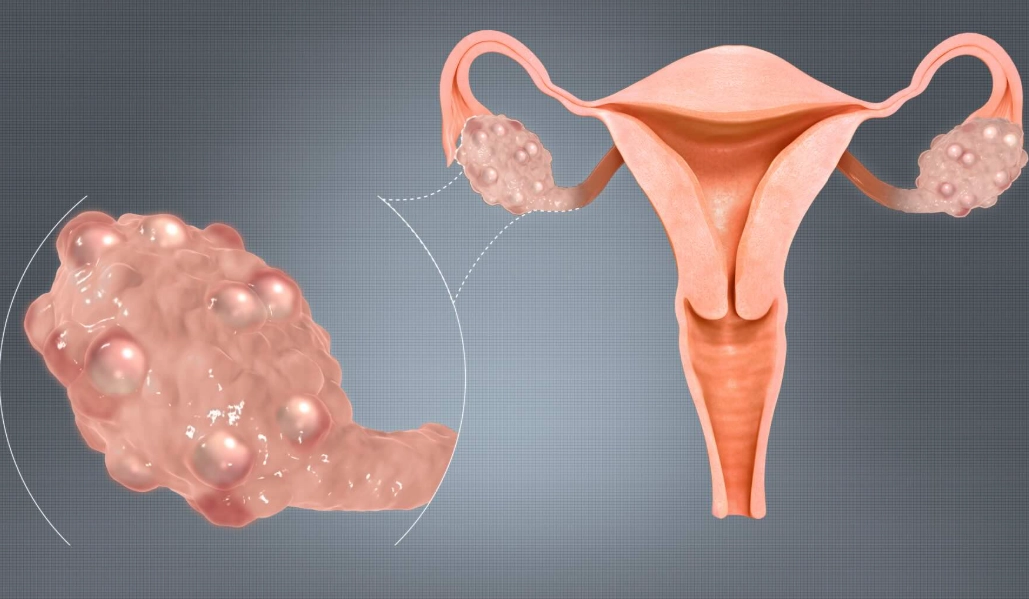
Step 3: Know What Tests to Ask About
- Pelvic Exam: The first step. A good clinician can sometimes feel a large cyst or mass.
- Transvaginal Ultrasound: The gold standard for imaging ovaries. It can see cysts, measure them, characterize their appearance (simple fluid vs. complex), and check blood flow. This is non-negotiable if symptoms persist.
- CA-125 Blood Test: A controversial one. It's a tumor marker, but it's not a screening test. It can be elevated in endometriosis, fibroids, infection, or even normal menstruation. It's most useful in conjunction with an ultrasound for women at high risk or with a concerning mass, not as a standalone answer.
Bring your symptom log to the appointment. It shows you're serious and helps cut through the noise.
Step 4: Interpret the Results (With Your Doctor)
Most ovarian cysts are functional (related to your cycle) and resolve on their own. The management plan depends on size, appearance, your symptoms, and your age. PCOS is diagnosed through a combination of symptoms, ultrasound, and blood tests for hormones like testosterone. A diagnosis of ovarian cancer involves a surgical biopsy.
Remember Sarah? Her cyst was benign, but it was causing significant symptoms. She had it removed laparoscopically. At her follow-up, she said, "I finally feel like myself again. I just wish I hadn't spent a year thinking it was all in my head." It wasn't in her head. It was in her pelvis.
For authoritative information, you can refer to resources from the CDC's page on PCOS, the National Cancer Institute's overview of ovarian cancer, and patient guides from the Mayo Clinic on ovarian cyst symptoms.
POST A COMMENT